Periodontal Disease Explained
Gum Disease. In scientific circles, Periodontal Disease, or Periodontitis. Pyorrhea, it used to be called. And when dental educators are discussing cases of broken-down dentitions with students, they often refer to patients with this condition as “periodontally involved.”
So, when two students in my dental school class started dating, it was especially funny when my classmate Dave arched his eyebrow and remarked, “Hey, did you hear that Sue and Ben are periodontally involved?”
Not their real names, but one of my favorite situational jokes.
What, then, is Periodontitis? It is a disease caused by bacteria in a very specific part of the mouth, the gums right alongside our teeth.
We don’t like to think about it, but germs are always attacking us. Oh, some bacteria are neutral, and some are even beneficial to us. Yet many germs mean us harm. We have many defenses. One of them is “turnover”: the natural shedding of skin cells, intestinal cells and so on. A germ on the skin of our arm or on the lining of our stomach finds itself perched precariously on shifting sands.
Teeth, though—teeth are different. They’re rock solid, they don’t shed surface layers and they’re not going anywhere anytime soon.
Bacteria can anchor themselves to teeth with a very different skill set than the skills it takes to live on a constantly shifting, shedding soft-tissue surface. Bacteria in the mouth form a biofilm, defined as layers of microorganisms and the polymers they secrete, all attached to a surface. In the mouth, we customarily refer to biofilm as plaque.
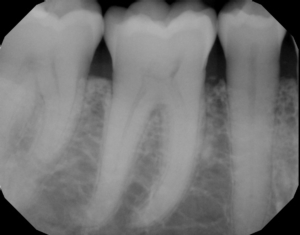
If left undisturbed, with the passage of time, plaque will spread and grow below the gum line. Toxins produced by the bacteria in plaque irritate the gums even more than the bacteria themselves. Those toxins stimulate a chronic inflammatory response in the gum tissues next to the teeth. It’s a battlefield, and although the cause is just—get rid of those harmful germs!—battlefields are always nasty places, and so the gum tissues and bone that support the teeth are broken down and destroyed. Gums separate from the teeth, forming pockets (spaces between the teeth and gums) that become infected. As periodontal disease progresses, the process accelerates and those pockets deepen faster and faster. Yet more jawbone is destroyed. The eventual result is tooth loss. Here’s a well-anchored molar (mine), compared to a molar in an absolutely breathtaking final stage of bone loss:
Are we driven by pain to seek care early in the periodontal disease process? Actually, no. Like many dangerous diseases–hypertension, glaucoma, diabetes–symptoms are minimal in the early and middle stages of periodontal disease.
From the American Academy of Periodontics website, https://www.perio.org/
Gum disease is often silent, meaning symptoms may not appear until an advanced stage of the disease. However, warning signs of gum disease include the following:
Red, swollen or tender gums or other pain in your mouth
Bleeding while brushing, flossing, or eating hard food
Gums that are receding or pulling away from the teeth, causing the teeth to look longer than before
Loose or separating teeth
Pus between your gums and teeth
Sores in your mouth
Persistent bad breath
A change in the way your teeth fit together when you bite
A change in the fit of partial dentures
Millions of people don’t know they have this serious infection that can lead to tooth loss if not treated.
Gums usually, though not always, do look different when they’re diseased. It is said that healthy gums have a stippled appearance, like an orange peel. Severe inflammation makes the gums all fluid-filled, and that stippling is lost:
On the next page we’ll have a look at the stats and risk factors for periodontal disease.
http://www.smilephiladelphian.com/periodontal-disease-risk-factors/